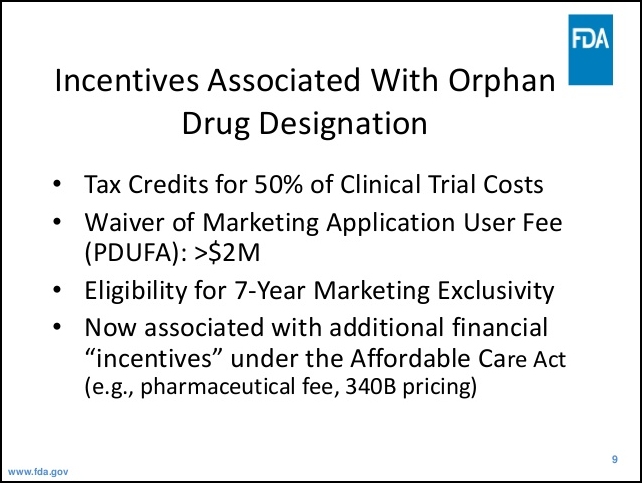
In “It Takes a Pandemic to Expose a Corrupt U.S. Healthcare System,” SA introduced you to Gilead, the drug company on track to make billions off its old war horse drug remdesivir. With the FDA at the end of its rope as the pandemic ravages the U.S. and facing growing pressure from the Trump administration, it formally designated remedesivir an “orphan “drug. A veritable bonanza giving Gilead a 7-year monopoly on sales of the drug. This market exclusivity extends to the sale of a generic. In addition, Gilead can price-gouge the drug to its heart’s content. These goodies courtesy of a friend in high places, Joe Grogan, Trump confidante and director of the U.S. Policy Center who used to be a lobbyist for — I kid you not —Gilead. (On April 30, Grogan announced he was resigning effective May 24).
News report of this hijacking resulted in outraged howls from critics and consumer groups forcing Gilead to petition the FDA to rescind the designation. But then the bombshell news. “Gilead’s remdesivir improves recovery time of coronavirus patients in NIH trial” (Washington Post, 4/30) and “Doctors have a new weapon in their fight to save lives…the FDA is expected to grant emergency approval for the drug. (NBC Nightly News, April 29, 2020)
The excitement was palpable. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases jettisoning his usual cautious, carefully nuanced messaging was taking a victory lap — “The data shows that remdesivir has a clear cut significant positive effect in diminishing the time to recover…It’s highly significant…What it has proven is that a drug can block this virus…a new standard of care.”
Not exactly. Results of a worldwide study of 1,100 patients show a drop of 31% in recovery time in the hospital— an impressive percent but in actual days the drop has reduced hospital stays from a little over two weeks (15 Days) to three days shy of two weeks. (11 days). In terms of patient deaths, the drop from 11.6% to 8% among remdesivir patients is not considered statistically significant.
Even CNN’s talking head Dr. Sanjay Gupta expressed surprise at Dr. Fauci’s enthusiasm. His response was more muted and a good deal more cautious advising a wait-and-see-approach.
Other experts were far less polite pointing out that the study compared patients taking remdesivir to patients taking a placebo. What the study lacked they noted was a control group of untreated patients. “They’ve squandered an unbelievable opportunity. It’s not going to tell us what to do with 80-year-olds with multiple comorbidities compared to 30-year-olds who are otherwise healthy. We’re still going to be foundering around in the dark, or at least in a dim room, when we could have learned more.” (Peter Bach, the director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Medical Center).
Even former FDA commissioner Dr. Scott Gottlieb, described in his official biography as an “American physician and investor,” and a poster boy for the revolving door between government and industry released a public statement awash in caution words — “[Result of the remdesivir study) isn’t a homerun…an important beginning…this drug does appear to be active against the virus and I think used properly in the course of early disease…it does appear that this drug has the potential to benefit some patients. Note his use of words like “appear” (used twice), and “potential” and his final comment, far from a ringing endorsement — the “potential” to benefit “some” patients.
But wait, there are other difficulties with this over-hyped study. It was “non-peer reviewed.” Does that make a difference? Peer reviews can validate the results of a study by holding it up to the scrutiny of other experts in the field to insure the results can be replicated. On the other hand, non-peer reviewed studies are not independently verified and thus might be relying on faulty data or other kinds of distortions to skew results. Although the value of replicating a study to confirm its results is a hot-button issue in the medical community, a drug with a demonstrated history of failure in other applications would seem to need external validation before touting it as a “new standard of care”
Remdesivir is no stranger to false promise. In a study out of China published in Lancet, the world’s leading independent general medical journal, the results pointed to a different conclusion — “[Remdesivir] did not significantly improve the time to clinical improvement, mortality, or time to clearance of virus in patients with serious COVID-19 compared with placebo.” While this trial was far from perfect, the Lancet describes it as “underpowered” (only 257 participants) and with a premature halt (lack of recruitable participants as the pandemic ebbed in China), its results, in sharp contrast to those coming out of the National Institutes of Health (NIH) remdesivir trial, should have been and were not publicized.
Dr. Fauci’s giddy response to the NIH trial results, so unlike his usual cautious optimism, is not the first time his words and demeanor suggest the compromises he’s had to make to appease a difficult boss. Several weeks ago, in televised remarks Dr. Fauci suggested that lives could have been saved if the Trump administration had acted faster to impose mandatory social distancing and country-wide closures of public spaces. When press reports surfaced that Trump was thinking of firing him, Fauci walked back his comment calling it “a poor choice of words…” hypothetical questions sometimes can get you into some difficulty.” When a reporter asked if Trump had suggested that “revision,” he appeared horrified —“Everything I do is voluntary. Please. Don’t even imply that.”

Not long after Fauci disavowed his remarks, Trump announced he had no intention of firing him.
Whether or not the trial results are overblown, one thing is clear. Should this be the magic bullet for COVID-19 treatment, Gilead is in for a multi-billion-dollar payday. With an administration full of capitalist privateers and political leadership on both sides of the aisle captive to the money and power of the pharmaceutical industry, the victims of Gilead’s greed and government indifference will be Americans. Italians, Spaniards, Canadians, Britishers and the citizens of virtually every other advanced country are the lucky ones. They won’t pay a dime to get life-saving treatment. That’s the difference between a national single payer healthcare system and the U.S. privatized, profit-oriented healthcare system.

The U.S. media in thrall to the oligarchs who control U.S. healthcare aren’t reporting what Americans will have to pay to save their lives. What they are talking up is Gilead’s announcement that it was donating 1.5 million vials of remdesivir—“the entirety of our supply through the early summer”—for use in clinical trials, compassionate use cases and beyond.
It’s an old corporate dodge. First convince consumers you feel their pain—a million and a half free doses ought to do the trick. Then while the media is agog with praise, the skyrocketing price will fly under the radar. Will the feds step up and stop the bleeding? Alex Azar, Health and Human Services Secretary and an ex-drug lobbyist, doesn’t see much hope for federal regulation of pharmaceutical price-gouging, at least when it comes to a COVID-19 vaccine — “We can’t control the price… this might not be affordable for all Americans.” Do you think he will respond differently to a treatment?
Here’s what Gilead’s CEO had to say about the potential price of remdesevir — “We deeply respect and appreciate the fact that when we get into millions of doses, we have to have a sustainable economic model that works here and that achieves access and affordability for patients around the world.” (CEO Daniel O’Dea, in a conference call to analysts 4/30/2020). Did he forget to mention that Gilead’s 2019 revenues were $22.45 billion?
That’s oligarch-speak for price-gouging and that’s the “sustainable economic model” so dear to what passes for the pharmaceutical industry’s heart.
For the American consumer stuck in a profit-making healthcare system, it’s the same old story. Means-tested treatment — if you’re poor, you die.
762 total views, 1 views today