
Welcome to the United States of profligacy where for four trillion dollars an underwhelming healthcare experience awaits. Worse yet when a major health crisis erupts, the richest country in the world is suddenly reduced to a pitiful giant. How could such a transformation occur?
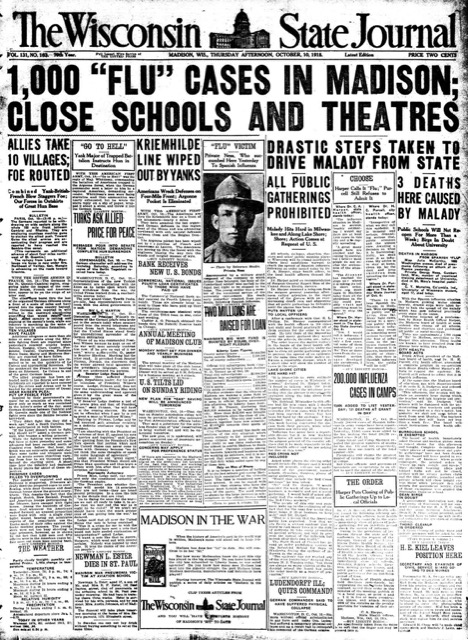
First let’s see how deep a hole the US has dug itself into. The last time the U.S. faced a global pandemic affecting millions was 100 years ago, the Spanish flu pandemic. Since that time, a vast array of lifesaving treatments have been developed. Spanish flu victims weren’t so lucky. It wasn’t until 1938 — 20 years after the outbreak — that Dr. Jonas Salk developed a Spanish flu vaccine. It took eight years for his vaccine to be approved for use in humans. Doctors were reduced to using non-medical treatments, many still in use today, such as isolation, quarantine, good personal hygiene, use of disinfectants, and limitations of public gatherings. Like today, these procedures were applied unevenly and, in some areas, totally ignored.
COVID vaccines became available in December 2020, less than a year after the first COVID cases surfaced. Antibiotics, important for treating COVID-related infections like pneumonia, were also a Godsend. They were not available in 1918 and left doctors helpless to treat thousands who eventually died of secondary infections.
Yet despite these revolutionary advances in medical treatments, America drew the short straw when it came to preventing or treating COVID. In 1918, best estimate is 28% of the population was infected with Spanish flu. By comparison, at the end of 2020, 31% had caught COVID and the number is on the rise as the Delta variant spreads. Death rates are another sore spot. Although the population in 1918 was about one-third what it is today, considering the ready availability of both vaccines and antibiotics, it is incomprehensible that the U.S. is only 20,000 deaths shy of the estimated death total from the Spanish flu.
Want to know how bad it really is? In 1918 total health care spending was a minuscule 3% of U.S. GDP, about $2 billion annually. On a per capita basis, that comes to $30/ person. Today, U.S. healthcare costs are 18% of GDP, a total of $4 trillion — an astounding and appalling $11,000/ person. What has $4 trillion brought the American people? First place in both the number of COVID cases and the number of deaths. That’s quite a feat for a country that has only 4% of the world’s population yet has managed a stunning 20% of its cases and deaths.
How could all hell have broken loose in a country blessed with the modern miracles of medicine? It wasn’t wonder drugs or even wonder vaccines that could have stopped the virus cold at the outset. Leave it to the weakest link in profit-making healthcare, preventive medicine. As the virus gained a toehold in the U.S. between late January and early March, healthcare “experts” at the top of the federal food chain were slow to mobilize a wide scale testing program. Their feeble attempts to develop an “American” test produced an unreliable basically useless test, while at the same time spurning offers of a reliable test from the World Health Organization — “[The C.D.C. did not think] we needed somebody else’s test.” [Dr. Anne Schuchat, CDC deputy director]. How wrong they were. While other countries mobilized businesses to perform tens of thousands of tests daily, in the U.S. fewer than 100 tests on average were being performed. Without the benefit of early identification, health authorities were helpless to stem the flow of “community spread” that kicked the pandemic into high gear. Result — a full blown public health crisis.
Speaking of America’s once-proud public health system, the U.S. has been in the thick of a public health crisis, independent of the pandemic, for many decades. As the fat cats in the private, profiteering medical community rake in buck bucks, the public suffers from a deterioration of public health services. Between 2002 and 2019 in both Republican and Democrat administrations, public health funding was cut along with 50,000 public health jobs. Then the pandemic struck. The U.S. was once again forced to play catch up with emergency funding. By that time, it was a case of too little too late to stem the worst of the crisis. In a $4 trillion dollar healthcare system, very little is going into the public health till. Where it is going is the answer to the question of the income inequality battering the U.S. economy.
Lack of well-funded local, state, and federal public health programs especially for low-income workers and people of color had already put the U.S. in the unenviable position of having the poorest health outcomes in the developed word. When the pandemic came calling, these same Americans were sitting ducks.
Leapfrogging from the inexcusable to the unforgivable is that pernicious system known as “just in time ordering” where the private overlords of U.S. healthcare order supplies like PPE, ventilators and other equipment needed to save lives only when supplies run out in order to enrich their own bottom lines. Since over 20% of U.S hospitals, over a third of the staff of emergency rooms around the country, 70% of nursing homes and almost half of doctors’ practices are privately held, the impetus by private owners to squeeze the very last dollar out of their investment is a U.S.special. When the pandemic hit and supply chains were disrupted, the chickens came home to roost as hospitals, emergency rooms and nursing homes that had failed to maintain inventories of critically needed supplies found themselves unable to care for their COVID patients. Thousands lost their lives so that an equity fund manager could build another yacht.
As the COVID crisis ratcheted up, public trust in the U.S. government’s commitment to affordable and life-saving healthcare fizzled. Having been bamboozled by the unaffordable prices of doctor’s visits and drugs, the public was in no mood to trust government officials who claimed that COVID testing and treatment were free (and indeed many who believed that yarn received humongous bills from doctors and hospitals). Others in frontline jobs without health insurance benefits waited until it was too late. That same lack of trust played a major role in vaccine hesitancy among a large swathe of Americans. A recent report estimates that 40% (over a quarter million) of U.S. COVID deaths could have been avoided if U.S. average death rates matched those of other industrialized nations with a national healthcare system. [Lancet Commission on Public Policy and Health].

U.S. healthcare which is perennially focused on the profit side of sickness was unprepared to confront a full-blown pandemic. That incompetence carried over to the care of patients as millions began flooding hospitals. All the ingredients of a recipe for disaster were present: the lack of widespread testing that could have contained the spread, a deteriorating, almost non-existent, public health sector that produced poorer health outcomes even before COVID than those of other developed countries and the decision by corporate bootleggers to cut inventories of life-saving supplies leaving hospitals and emergency rooms scrambling to make up for their greed.
It wasn’t all gloom and doom. In the executive suites of big Pharma, health insurance companies, equity firms with a big stake in hospitals, emergency rooms and doctors’ practices, the champagne was flowing. 61 new billionaires emerged from the healthcare field in 2020—of those 40 were directly involved in marketing goods and services for the pandemic.
America’s private profiteering health care system has endured through two major pandemics costing over one and one half million Americans their lives. During the Spanish flu epidemic, accusations of price gouging and kickbacks were common. Sound familiar?
